During a glaucoma eye exam, there are a number of tests performed, But knowing what these test are and how to interpret the results is very important for the glaucoma patient. In this section, we explore the basic tests and the corresponding results which most ophthalmologists or glaucoma specialists will perform.
Introduction Often there are no symptoms with glaucoma until damage is irreversible and there is considerable loss of optic nerve tissue. It is estimated than many do not get routine eye examinations and therefore, are not being screened for the possibility of glaucoma or ocular hypertension. The earliest signs indicating glaucoma or 'glaucoma suspect' seen by an optometrist, clinic, or ophthalmologist are eye pressures which run higher than the upper range of 21 mm Hg. This is usually an indication when your doctor may 'dig deeper' with other testing and exams. In the following sections, the basic glaucoma eye exams are introduced. Eye Pressure Measurements - Tonometry 
A common part of any eye exam usually involves a measurement of intraocular pressure in the eye.
There are different types of tonometers such as the air puff Reichert used by many of our FitEyes members who practice self tonometry. These instruments may also be used with routine screening by an optometrist. However, the type of tonometer that would be used during a glaucoma exam by an ophthalmologist would probably be a Goldman Applanation Tonometer or GAT. Because the instrument must come into contact with the eye for the ‘applanation’, numbing drops are first applied so that the measurement procedure is not uncomfortable. Therefore, the doctor or technician will first apply these numbing drops to your eyes before taking the measurements.
The range for normal pressure is conventionally 12- 22 mm Hg, but depending on other factors from the final array of tests results, a doctor may sometimes decide to proceed with treatment based on a lower than maximum pressure of this range. Alternately, sometimes if the pressures run higher than 22 mmHG, the doctor may not prescribe treatment if there are no other risk factors. In this case a diagnosis of ocular hypertension (OHT) or glaucoma suspect is given. It should be noted here that we at FitEyes believe that only relying on routine doctor visits for eye pressure determination does not present a fully accurate picture.Therefore, the article Why You Should Monitor Your IOP should also be read.
Visual Field Perimetry Tests
The retina, which is the light-sensitive nerve tissue at the back of the eye, is composed of receptors, "photoreceptors," that change light energy
into electrical energy. The central area of the retina is the most sensitive, which allows us to see more clearly the objects directly in front of us. How much we can see from central focus to our periphery, is known as our visual field. The photoreceptors around our retina pick up signals by special nerve cells known as ganglion cells, pass on the signal from these to the optic nerve, and then finally to the brain. Any impairment in the function of these cells will effect that portion of the retina's visual field, which will then be less sensitive to the corresponding stimuli in that area of the field.
The central area of the retina is the most sensitive to light, and we see best what is directly in front of us. The more peripheral areas of the retina are less sensitive to light, but they allow us to see, though less clearly, objects off to the side or above or below 'straight-ahead' vision. Just how much we can see of the world around us is known as our visual field. Each part of the retina "sees" a particular part of the visual field. Each photoreceptor’s signal is then picked up by a special nerve cell called a ganglion cell. The ganglion cells then transmit the signal via the optic nerve to the brain, allowing us to see. Thus, each ganglion cell is responsible for "connecting" a portion of the retina to the brain. Any disruption in the function of these cells will block the signal’s transmission and render that portion of the retina (and the accompanying visual field) less sensitive to light.
With these facts in mind, a standard glaucoma test called the Visual Field (or Perimetry) is used. It helps determine and map the functioning level of these cells. However, this is just one in a series of tests, because there can be changes and deterioration to these nerve cells before the visual field detects them. In the VF test, one is instructed to fixate each eye individually on a center light, and then press a button as a series of random lights are flashed in different positions (and varying intensity) around the periphery of the visual field. One standard test is the Humphrey automated perimetry, and fortunately, this test has been refined such that it is not as arduous and lengthy as in times past, and can now take from only 3 to 8 minutes for completion.
Some preliminary factors are important in determining the test results, and among these are the patient's age and visual acuity (which for other reasons besides glaucoma may effect results). A patient can see these factors upon examination of the test results output.
The following are the factors used by the test to determine reliability of results:
- Fixation Losses – This number shown on the top left of the test, determines how often the eye has moved off of the center target.
- False Positive Errors – This reflects the percentage of times which the patient pressed the button when no flash was present. It is common for patients wishing to perform maximally on test, to 'imagine' seeing flashes when none are present, and the stress alone of taking the test can rev up the adrenalin levels thus causing over reaction. The test will often create false sounds when no light flash is present in order to properly gauge the patient's reaction etc.
- False Negative Errors – A light may be repeated at the same position but at different intensities. Depending of the intensity level noted at the same position, the reliability of the test may be adjusted accordingly. However, it is normal for those with glaucoma to have fluctuations at the edge of their visual field, so not all such errors are a problem.
Refer now to the quadrant sections of the Sample Visual Field:
- Retinal Sensitivity - The numbers noted on the printout of the quadrants represent the intensity of the light needed for detection at that location. Therefore, a higher number represents a score meaning that a lower light level could be detected. Correspondingly, a lower number means a higher intensity of light was needed before detection. Therefore, a higher number is better.
- Dark vs lighter areas – Corresponding to the retinal sensitivity, a lighter shades indicate a higher score (greater detection) in a specific area of the perimetry, and a lower score of the RS is indicated by darker areas. Of course, the central blind spot is normal for everyone, and is indicated on 'x' of the diagram.
- Dark blocks – On this part of the output, dark blocks indicate areas where the person deviated from the normal vision expected for his or her age.
Links for more indepth study:
Youtube videos:
Fundus and Optic Nerve Exams
The fundus is the interior surface of the eye, opposite the lens, and includes the retina, optic disc, blood vessels, macula and fovea, and posterior pole. An examination of the fundus is usually done after first applying mydriatic dilation drops which enlarge the pupil opening, and thus allowing a better view of these structures. The instruments used for fundus examination include ophthalmoscope or a fundus camera. The camera has the advantage of allowing for better documentation of any changes to these structures over time. In addition, a '
Slit Lamp' is also commonly used for glaucoma eye exams. It is a highly magnifying instrument which can provide three dimensional views of anterior eye disorders such as cataracts, and by using a special lens, the drainage angle and posterior problems such as thinning of the optic nerve tissue can be determined.
Gonioscopy
Gonioscopy allows exclusive examination of the front or anterior part of the eye from the iris forward to the cornea. The main test objective is to examine the drainage canal, and this is done via noting whether the angle formed by the iris is open, narrow, or closed. If the angle is not open, this can put one at risk for a blockage of aqueous fluid moving from around the pupil outward towards the drain. This blockage called angle closure and/or pupillary block can cause very high pressure spikes which can become an emergency situation and put on at risk for optic nerve damage.
A gonioscopy can also determine if there is any scarring around the trabecula, and the degree of pigmentation or exfoliation which could interfere with proper functioning of the drainage mechanism. This test can also check other less common conditions such as plateau iris.
The procedure is painless because the eye is first numbed with special drops, and only takes about 5 minutes. It consists of a special lens that is can be placed in front of the slit lamp or held separately.
Pachymetry - Measuring the Central Thickness of the Cornea
The cornea or outer surface of the eye can vary in thickness with the average CCT (or Central Corneal Thickness) in the range of 555 microns.
Less thickness than this has been implicated in increased risk for glaucoma in some studies. Additionally, it has been traditionally thought that an increased thickness can yield an over estimated pressure reading on GAT tonometry (as revealed in the ocular hypertension studies), and a thinner than average CCT can report a lower reading which may need to be adjusted upwards.
However, newer research points to other properties of the cornea such as corneal hysteresis or CH, as being more important than simple thickness. Newer tonometers like the Reichert 7CR will give both an IOPg (which is the GAT equivalent measurement) and a IOPcc, which is the corneal compensated pressure that factors in the hysteresis and other bio mechanical characteristics. An IOPcc which is lower than the IOPg is considered a lower risk factor. As an example of the limitations of relying on CCT measurements alone, some have been found with very thick CCTs but also had lower CH and higher IOPcc!
In summary, the actual pachymetry test, is a simple, quick and painless exam involving a small ultrasonic device which touches the cornea. It is also advantageous at gauging the health of other corneal conditions.
Optical Coherence Tomography (OCT)
Sample OCT scan: https://eyeguru.org/essentials/interpreting-octs/
Referring to the above link, OCT is a newer test within the past several years which can measure the thickness of the Retinal Nerve Fiber Layers (RNFL) composing the optic nerve. In this test, a laser light is used to scan the internal structures of retina, and in the case of glaucoma, early changes to the nerve fiber layer thickness can be revealed even before visual field or other tests detect changes. The doctor will use the results of the test to determine changes in the quadrants of the optic nerve structure.
Referring to the above link, it can be seen in this sample exam that the results are divided into four quadrants. The color designations are: 1) Green - Within normal limits of the general population for RNFL. 2) Yellow - Borderline for RNFL. 3) Red - Outside normal limits for RNFL and therefore, suggestive of optic nerve damage in representative area.
It can be seen from this sample scan, that there is a dark line which represents the RNFL for this patient, and that there are quadrant areas where this line crosses into the 'outside normal limits' area. Doctors can use these results in association with the visual field test to determine how RNFL regions correlate with test scores of VF regions. This helps the doctor develop a more accurate picture of the patients condition.
Cup to Disk Ratio
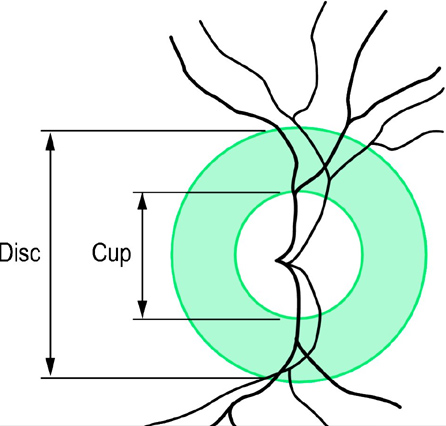 .....
.....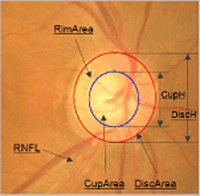 In the preceding tests from which there is an examination of the optic nerve, the doctor will note a parameter usually referred to as 'cup to disc ratio' and will determine this by visual examination or by fundus photographs. As the branches of the optic nerve emerge from the back of the eyes, (and from a frontal view), they will form a cylindrical disk. This is the area where the blind spot is located, which is the area where the optic nerve and blood vessels enter the retina. Referring to the diagram above and to the detail overlays of the optic nerve fundus photo, the cup is the centermost portion of the disk and is the area devoid of neuro retinal tissue. An easy way to picture this is to imagine a donut with the center portion being the hole and the surrounding nerve and blood vessels being the disk. With the progression of nerve cell loss, the center 'hole' area becomes larger and so the cup to disk ratio becomes greater. Therefore, indications of pathology are primarily determined when the cup-to-disk ratio becomes greater or if it is larger than 0.5 (the cup occupying 1/2 the disk etc.). Note however, that some people have a larger cup-to-disk ratio naturally, so progression or 'cupping,' asymmetry of one eye ratio to another, or changes of coloration etc. are better determinations of glaucoma progression than a one time C:D determination. A glaucoma patient will often hear the term 'cupping' and this relates to above description of nerve loss. Eye Chart and Refraction Testing
In the preceding tests from which there is an examination of the optic nerve, the doctor will note a parameter usually referred to as 'cup to disc ratio' and will determine this by visual examination or by fundus photographs. As the branches of the optic nerve emerge from the back of the eyes, (and from a frontal view), they will form a cylindrical disk. This is the area where the blind spot is located, which is the area where the optic nerve and blood vessels enter the retina. Referring to the diagram above and to the detail overlays of the optic nerve fundus photo, the cup is the centermost portion of the disk and is the area devoid of neuro retinal tissue. An easy way to picture this is to imagine a donut with the center portion being the hole and the surrounding nerve and blood vessels being the disk. With the progression of nerve cell loss, the center 'hole' area becomes larger and so the cup to disk ratio becomes greater. Therefore, indications of pathology are primarily determined when the cup-to-disk ratio becomes greater or if it is larger than 0.5 (the cup occupying 1/2 the disk etc.). Note however, that some people have a larger cup-to-disk ratio naturally, so progression or 'cupping,' asymmetry of one eye ratio to another, or changes of coloration etc. are better determinations of glaucoma progression than a one time C:D determination. A glaucoma patient will often hear the term 'cupping' and this relates to above description of nerve loss. Eye Chart and Refraction Testing
In the standard eye chart test, you are asked to cover one eye and read as may lines of texts on the eye chart as possible. This will gauge your visual acuity and also help determine whether you are nearsighted (myopia), farsighted (hyperopia) or possibly have astigmatism. A further test often used is the auto refractometer which will actually measure the nearsightedness or farsightedness of your eyes and assigns a number (given in diopters). This test has value because myopia is considered to be a risk factor for glaucoma, and extreme hyperopia can sometimes be a contributing factor in narrow angles because of the shorter axial length contributing to crowding in the anterior eye structures. In a common refractometer test, you are asked to look into an instrument and stare at a balloon or similar object. The test is very quick and accurate.
In summary, a variety of tests are administered by an ophthalmologist or glaucoma specialist to determine the nature of the specific form of condition and to prescribe the optimal treatments. Routine exams also provide benchmarks so that doctors can see changes. This is important because it is often the changes rather than specific isolated test results which determine whether glaucoma is progressing.

 into electrical energy. The central area of the retina is the most sensitive, which allows us to see more clearly the objects directly in front of us. How much we can see from central focus to our periphery, is known as our visual field. The photoreceptors around our retina pick up signals by special nerve cells known as ganglion cells, pass on the signal from these to the optic nerve, and then finally to the brain. Any impairment in the function of these cells will effect that portion of the retina's visual field, which will then be less sensitive to the corresponding stimuli in that area of the field.
into electrical energy. The central area of the retina is the most sensitive, which allows us to see more clearly the objects directly in front of us. How much we can see from central focus to our periphery, is known as our visual field. The photoreceptors around our retina pick up signals by special nerve cells known as ganglion cells, pass on the signal from these to the optic nerve, and then finally to the brain. Any impairment in the function of these cells will effect that portion of the retina's visual field, which will then be less sensitive to the corresponding stimuli in that area of the field.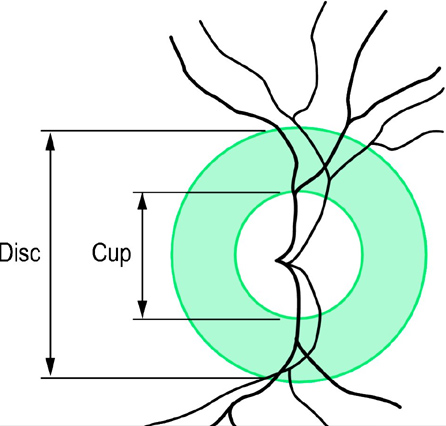 .....
.....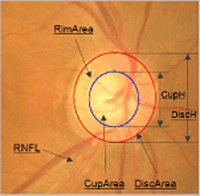 In the preceding tests from which there is an examination of the optic nerve, the doctor will note a parameter usually referred to as 'cup to disc ratio' and will determine this by visual examination or by fundus photographs. As the branches of the optic nerve emerge from the back of the eyes, (and from a frontal view), they will form a cylindrical disk. This is the area where the blind spot is located, which is the area where the optic nerve and blood vessels enter the retina. Referring to the diagram above and to the detail overlays of the optic nerve fundus photo, the cup is the centermost portion of the disk and is the area devoid of neuro retinal tissue. An easy way to picture this is to imagine a donut with the center portion being the hole and the surrounding nerve and blood vessels being the disk. With the progression of nerve cell loss, the center 'hole' area becomes larger and so the cup to disk ratio becomes greater. Therefore, indications of pathology are primarily determined when the cup-to-disk ratio becomes greater or if it is larger than 0.5 (the cup occupying 1/2 the disk etc.). Note however, that some people have a larger cup-to-disk ratio naturally, so progression or 'cupping,' asymmetry of one eye ratio to another, or changes of coloration etc. are better determinations of glaucoma progression than a one time C:D determination. A glaucoma patient will often hear the term 'cupping' and this relates to above description of nerve loss. Eye Chart and Refraction Testing
In the preceding tests from which there is an examination of the optic nerve, the doctor will note a parameter usually referred to as 'cup to disc ratio' and will determine this by visual examination or by fundus photographs. As the branches of the optic nerve emerge from the back of the eyes, (and from a frontal view), they will form a cylindrical disk. This is the area where the blind spot is located, which is the area where the optic nerve and blood vessels enter the retina. Referring to the diagram above and to the detail overlays of the optic nerve fundus photo, the cup is the centermost portion of the disk and is the area devoid of neuro retinal tissue. An easy way to picture this is to imagine a donut with the center portion being the hole and the surrounding nerve and blood vessels being the disk. With the progression of nerve cell loss, the center 'hole' area becomes larger and so the cup to disk ratio becomes greater. Therefore, indications of pathology are primarily determined when the cup-to-disk ratio becomes greater or if it is larger than 0.5 (the cup occupying 1/2 the disk etc.). Note however, that some people have a larger cup-to-disk ratio naturally, so progression or 'cupping,' asymmetry of one eye ratio to another, or changes of coloration etc. are better determinations of glaucoma progression than a one time C:D determination. A glaucoma patient will often hear the term 'cupping' and this relates to above description of nerve loss. Eye Chart and Refraction Testing
